|
Overview
 They make it possible for us to walk, run, and stand. With over two dozen bones, your feet are really a masterpiece of engineering. But sometimes even the best made things have flaws. One common problem is to have flatfeet, or fallen arches. Causes Flat feet in adults can arise from a variety of causes. Here are the most common. An abnormality that is present from birth, stretched or torn tendons, damage or inflammation of the posterior tibial tendon (PTT), which connects from your lower leg, along your ankle, to the middle of the arch, broken or dislocated bones. Some health conditions, such as rheumatoid arthritis, Nerve problems. Other factors that can increase your risk include obesity, diabetes, ageing and Pregnancy. Symptoms The majority of children and adults with flexible flatfeet never have symptoms. However, their toes may tend to point outward as they walk, a condition called out-toeing. A person who develops symptoms usually complains of tired, aching feet, especially after prolonged standing or walking. Symptoms of rigid flatfoot vary depending on the cause of the foot problem. Congenital vertical talus. The foot of a newborn with congenital vertical talus typically has a convex rocker-bottom shape. This is sometimes combined with an actual fold in the middle of the foot. The rare person who is diagnosed at an older age often has a "peg-leg" gait, poor balance and heavy calluses on the soles where the arch would normally be. If a child with congenital vertical talus has a genetic disorder, additional symptoms often are seen in other parts of the body. Tarsal coalition. Many people have no symptoms, and the condition is discovered only by chance when an X-ray of the foot is obtained for some other problem. When symptoms occur, there is usually foot pain that begins at the outside rear of the foot. The pain tends to spread upward to the outer ankle and to the outside portion of the lower leg. Symptoms usually start during a child's teenage years and are aggravated by playing sports or walking on uneven ground. In some cases, the condition is discovered when a child is evaluated for unusually frequent ankle sprains. Lateral subtalar dislocation. Because this often is caused by a traumatic, high-impact injury, the foot may be significantly swollen and deformed. There also may be an open wound with bruising and bleeding. Diagnosis If your child has flatfeet, his or her doctor will ask about any family history of flatfeet or inherited foot problems. In a person of any age, the doctor will ask about occupational and recreational activities, previous foot trauma or foot surgery and the type of shoes worn. The doctor will examine your shoes to check for signs of excessive wear. Worn shoes often provide valuable clues to gait problems and poor bone alignment. The doctor will ask you to walk barefoot to evaluate the arches of the feet, to check for out-toeing and to look for other signs of poor foot mechanics. The doctor will examine your feet for foot flexibility and range of motion and feel for any tenderness or bony abnormalities. Depending on the results of this physical examination, foot X-rays may be recommended. X-rays are always performed in a young child with rigid flatfeet and in an adult with acquired flatfeet due to trauma. bestshoelifts Non Surgical Treatment Get shoes made for walking or running. One way to support your arch is to wear good-quality running or walking shoes, says Dr. Gastwirth. "These shoes generally provide good support to the foot." Add support. The top-of-the-line arch support is an orthotic insole, which may cost $900 or more and must be custom-made. "But many people with sore arches will get relief with over-the-counter arch supports for about $10," suggests Judith Smith, M.D., assistant professor of orthopedic surgery at Emory University School of Medicine in Atlanta. "The thing to remember about arch supports is that your shoe must have enough depth to accommodate them. Otherwise, you'll get a lot of rubbing on the top of your foot, or your heel will come out of the shoe." Most mens shoes are deep enough to accommodate the insoles; women should take their shoes with them to the drugstore when buying the insoles to ensure a good fit. If your heels are high, keep them wide. High heels may be your Achilles' heel--especially if you wear them constantly. "Flatter shoes are no doubt better," says Dr. Sanfilippo. Flat heels help prevent fallen arches and are kinder to your feet if fallen arches have already occurred. "If you must wear high heels, choose styles with a wide heel. Stay away from stiletto heels." Surgical Treatment  Generally one of the following procedures is used to surgically repair a flat foot or fallen arch. Arthrodesis. One or more of your bones in the foot or ankle are fused together. Osteotomy. Correcting alignment by cutting and reshaping a bone. Excision. Removing a bone or a bone spur. Synovectomy. Cleaning the sheath that covers the tendon. Tendon transfer. Using a piece of one tendon to lengthen or replace another. Arthroereisis. placing a small device in the subtalar joint to limit motion. For most people, treatment is successful, regardless of the cause, although the cause does does play a major role in determining your prognosis. Some causes do not need treatment, while others require a surgical fix. After Care Patients may go home the day of surgery or they may require an overnight hospital stay. The leg will be placed in a splint or cast and should be kept elevated for the first two weeks. At that point, sutures are removed. A new cast or a removable boot is then placed. It is important that patients do not put any weight on the corrected foot for six to eight weeks following the operation. Patients may begin bearing weight at eight weeks and usually progress to full weightbearing by 10 to 12 weeks. For some patients, weightbearing requires additional time. After 12 weeks, patients commonly can transition to wearing a shoe. Inserts and ankle braces are often used. Physical therapy may be recommended. There are complications that relate to surgery in general. These include the risks associated with anesthesia, infection, damage to nerves and blood vessels, and bleeding or blood clots. Complications following flatfoot surgery may include wound breakdown or nonunion (incomplete healing of the bones). These complications often can be prevented with proper wound care and rehabilitation. Occasionally, patients may notice some discomfort due to prominent hardware. Removal of hardware can be done at a later time if this is an issue. The overall complication rates for flatfoot surgery are low. Overview
 Your foot is made up of 26 bones, 33 joints, and more than 100 tendons. The heel is the largest bone in your foot. If you overuse or injure your heel, you may experience heel pain. This can range from mild to disabling. In many cases, if you have heel pain, you will need a doctor to diagnose the cause. Causes In our pursuit of healthy bodies, pain can be an enemy. In some instances, however, it is of biological benefit. Pain that occurs right after an injury or early in an illness may play a protective role, often warning us about the damage we've suffered. When we sprain an ankle, for example, the pain warns us that the ligament and soft tissues may be frayed and bruised, and that further activity may cause additional injury. Pain, such as may occur in our heels, also alerts us to seek medical attention. This alert is of utmost importance because of the many afflictions that contribute to heel pain. Symptoms Initially, this pain may only be present when first standing up after sleeping or sitting. As you walk around, the muscle and tendon loosen and the pain goes away. As this problem progresses, the pain can be present with all standing and walking. You may notice a knot or bump on the back of the heel. Swelling may develop. In some cases, pressure from the back of the shoe causes pain. Diagnosis The diagnosis of plantar fasciitis is generally made during the history and physical examination. There are several conditions that can cause heel pain, and plantar fasciitis must be distinguished from these conditions. Pain can be referred to the heel and foot from other areas of the body such as the low back, hip, knee, and/or ankle. Special tests to challenge these areas are performed to help confirm the problem is truly coming from the plantar fascia. An X-ray may be ordered to rule out a stress fracture of the heel bone and to see if a bone spur is present that is large enough to cause problems. Other helpful imaging studies include bone scans, MRI, and ultrasound. Ultrasonographic exam may be favored as it is quick, less expensive, and does not expose you to radiation. Laboratory investigation may be necessary in some cases to rule out a systemic illness causing the heel pain, such as rheumatoid arthritis, Reiter's syndrome, or ankylosing spondylitis. These are diseases that affect the entire body but may show up at first as pain in the heel. Non Surgical Treatment When consulting a doctor about heel pain, a patient can expect to be questioned about their level of pain, how long they?ve been experiencing it, and which activities aggravate or alleviate the condition. The doctor may order x-rays, a physical therapy regimen, or refer the afflicted individual to an orthopedic specialist for further examination. The doctor may attempt to recreate conditions that cause the heel pain to flare up in order to study reaction and cause in the patient, but this will be temporary and the doctor will stop this test at the request of the patient. A patient with heel pain may also be fitted with special inserts for their shoes to help correct arch and heel problems that cause pain. Heel problems can range from the mildly irritating to the nearly devastating, but proper prevention in care will help keep each step pain free. Advanced orthopedics, pain management, and technologically-honed surgical techniques ensure that no patient needs to suffer with the discomfort of heel pain and the restrictions it imposes on an active lifestyle. Surgical Treatment Extracorporeal shockwave therapy (EST) is a fairly new type of non-invasive treatment. Non-invasive means it does not involve making cuts into your body. EST involves using a device to deliver high-energy soundwaves into your heel. The soundwaves can sometimes cause pain, so a local anaesthetic may be used to numb your heel. It is claimed that EST works in two ways. It is thought to have a "numbing" effect on the nerves that transmit pain signals to your brain, help stimulate and speed up the healing process. However, these claims have not yet been definitively proven. The National Institute for Health and Care Excellence (NICE) has issued guidance about the use of EST for treating plantar fasciitis. NICE states there are no concerns over the safety of EST, but there are uncertainties about how effective the procedure is for treating heel pain. Some studies have reported that EST is more effective than surgery and other non-surgical treatments, while other studies found the procedure to be no better than a placebo (sham treatment). heel pain cure Prevention  You can reduce the risk of heel pain in many ways, including. Wear shoes that fit you properly with a firm fastening, such as laces. Choose shoes with shock-absorbent soles and supportive heels. Repair or throw out any shoes that have worn heels. Always warm up and cool down when exercising or playing sport, include plenty of slow, sustained stretches. If necessary, your podiatrist will show you how to tape or strap your feet to help support the muscles and ligaments. Shoe inserts (orthoses) professionally fitted by your podiatrist can help support your feet in the long term. Overview
Surgeries for LLD are designed to do one of three general things ? shorten the long leg, stop or slow the growth of the longer or more rapidly growing leg, or lengthen the short leg. Stopping the growth of the longer leg is the most commonly utilized of the three approaches and involves an operation known as an epiphysiodesis , in which the growth plate of either the lower femur or upper tibia is visualized in the operating room using fluoroscopy (a type of real-time radiographic imaging) and ablated , which involves drilling into the region several times, such that the tissue is no longer capable of bone growth. Because the epiphyseal growth capabilities cannot be restored following the surgery, proper timing is crucial. Usually the operation is planned for the last 2 to 3 years of growth and has excellent results, with children leaving the hospital within a few days with good mobility. However, it is only appropriate for LLD of under 5cm.  Causes The causes of LLD may be divided into those that shorten a limb versus those that lengthen a limb, or they may be classified as affecting the length versus the rate of growth in a limb. For example, a fracture that heals poorly may shorten a leg slightly, but does not affect its growth rate. Radiation, on the other hand, can affect a leg's long-term ability to expand, but does not acutely affect its length. Causes that shorten the leg are more common than those that lengthen it and include congenital growth deficiencies (seen in hemiatrophy and skeletal dysplasias ), infections that infiltrate the epiphysis (e.g. osteomyelitis ), tumors, fractures that occur through the growth plate or have overriding ends, Legg-Calve-Perthes disease, slipped capital femoral epiphysis (SCFE), and radiation. Lengthening can result from unique conditions, such as hemihypertrophy , in which one or more structures on one side of the body become larger than the other side, vascular malformations or tumors (such as hemangioma ), which cause blood flow on one side to exceed that of the other, Wilm's tumor (of the kidney), septic arthritis, healed fractures, or orthopaedic surgery. Leg length discrepancy may arise from a problem in almost any portion of the femur or tibia. For example, fractures can occur at virtually all levels of the two bones. Fractures or other problems of the fibula do not lead to LLD, as long as the more central, weight-bearing tibia is unaffected. Because many cases of LLD are due to decreased rate of growth, the femoral or tibial epiphyses are commonly affected regions. Symptoms LLD do not have any pain or discomfort directly associated with the difference of one leg over the other leg. However, LLD will place stress on joints throughout the skeletal structure of the body and create discomfort as a byproduct of the LLD. Just as it is normal for your feet to vary slightly in size, a mild difference in leg length is normal, too. A more pronounced LLD, however, can create abnormalities when walking or running and adversely affect healthy balance and posture. Symptoms include a slight limp. Walking can even become stressful, requiring more effort and energy. Sometimes knee pain, hip pain and lower back pain develop. Foot mechanics are also affected causing a variety of complications in the foot, not the least, over pronating, metatarsalgia, bunions, hammer toes, instep pain, posterior tibial tendonitis, and many more. Diagnosis The only way to decipher between anatomical and functional leg length inequalities (you can have both) is by a physical measurement and series of biomechanical tests. It is actually a simple process and gets to the true cause of some runner?s chronic foot, knee, hip and back pain. After the muscles are tested and the legs are measured it may be necessary to get a special X-ray that measures both of your thighs (Femurs) and legs (Tibias). The X-ray is read by a medical radiologist who provides a report of the actual difference down to the micrometer leaving zero room for error. Once the difference in leg length is known, the solution becomes clear. Non Surgical Treatment The treatment of LLD depends primarily on the diagnosed cause, the age of the patient, and the severity of the discrepancy. Non-operative treatment is usually the first step in management and, in many cases, LLD is mild or is predicted to lessen in the future, based on growth rate estimates in the two legs. In such cases, no treatment may be necessary or can be delayed until a later stage of physical maturity that allows for clearer prognostic approximation. For LLD of 2cm to 2.5cm, treatment may be as simple as insertion of a heel lift or other shoe insert that evens out leg lengths, so to speak. For more severe cases, heel lifts can affect patient comfort when walking, decrease ankle stability, and greatly increase the risk of sprains. For infants with congenital shortening of the limb, a prosthetic ? often a custom-fit splint made of polypropylene ? may be successful in treating more severe LLD without surgery. In many instances, however, a surgical operation is the best treatment for LLD.  shoe lifts for height Surgical Treatment Many people undergo surgery for various reasons - arthritis, knee replacement, hip replacement, even back surgery. However, the underlying cause of leg length inequality still remains. So after expensive and painful surgery, follow by time-consuming and painful rehab, the true culprit still remains. Resuming normal activities only continues to place undue stress on the already overloaded side. Sadly so, years down the road more surgeries are recommended for other joints that now endure the excessive forces. Overview
 Morton's neuroma is named after Dr Morton who first described this condition in 1876. It is sometimes called Morton's metatarsalgia or interdigital neuroma. It is a condition that affects one of the common plantar digital nerves that run between the long bones (metatarsals) in the foot. It most commonly affects the nerve between the third and fourth metatarsal bones, causing pain and numbness in the third and fourth toes. It can also affect the nerve between the second and third metatarsal bones, causing symptoms in the second and third toes. Morton's neuroma rarely affects the nerve between the first and second, or between the fourth and fifth, metatarsal bones. It tends to affect only one foot. It is rare to get two neuromas at the same time in the same foot. Morton's neuroma is named after Dr Morton who first described this condition in 1876. It is sometimes called Morton's metatarsalgia or interdigital neuroma. It is a condition that affects one of the common plantar digital nerves that run between the long bones (metatarsals) in the foot. It most commonly affects the nerve between the third and fourth metatarsal bones, causing pain and numbness in the third and fourth toes. It can also affect the nerve between the second and third metatarsal bones, causing symptoms in the second and third toes. Morton's neuroma rarely affects the nerve between the first and second, or between the fourth and fifth, metatarsal bones. It tends to affect only one foot. It is rare to get two neuromas at the same time in the same foot.Causes Morton's Neuroma is a caused by pressure, abnormal function/motion or an imbalance in the structure of the foot such as flat feet, that causes an abnormal pressure on the structures and the nerves in the ball of the foot. It most commonly affects the nerve that goes to the 2nd 3rd or 4th toes. The squeezing of the nerve from abnormal motion leads to a protective thickening of the sheath that protects the nerve. Symptoms of Morton's Neuroma often occur during or after activities that cause a sidewards squeezing of the ball of the foot or from pressure such as walking, standing, or playing sport. Since squeezing is a common cause of the condition, shoes such as pointed toes or high heels can often lead to a neuroma. Shoes that are constricting, even tight sneakers, can pinch the nerve between the toes, causing inflammation and pain. Symptoms Pain is usually increased by forefoot weight bearing activities (such as running), with narrow-fitting footwear, or with high heeled shoes. It is usually painful to firmly touch the affected region and, in chronic cases, pain and sometimes an audible click, may be heard when squeezing the foot and toes together with the hand. Often a localized area of swelling may be evident at the site of injury. Diagnosis The diagnosis of interdigital neuroma is usually made by physical examination and review of the patient's medical history.MRI ad High Definition Ultrasound examination may be useful to confirm the diagnoses however they may still not be 100% reliable. The commonest reason for this is de to natural substances present in between the metatarsal heads and between the fat pad and the intermetatarsal ligament. These natural substances i.e. bursa, fat, capsular thickening and even bony growths, can all be a factor in the impingement process and may need to be surgically cleared. Non Surgical Treatment You may be able to treat this problem at home. Avoid wearing tight, pointy, or high-heeled shoes. Choose well-fitted shoes with plenty of room for your toes. Put ice or a cold pack on the area for 10 to 15 minutes at a time. Put a thin cloth between the ice and your skin. Take anti-inflammatory medicines to reduce pain and swelling. These include ibuprofen (such as Advil or Motrin) and naproxen (such as Aleve). Rest your feet when you can. Reduce activities that put pressure on the toes, such as racquet sports or running. Try massaging your foot to relax the muscles around the nerve. If these steps do not relieve your symptoms, your doctor may have you use special pads or devices that spread the toes to keep them from squeezing the nerve. In some cases, a doctor may give a steroid shot to reduce swelling and pain. If these treatments do not help, your doctor may suggest surgery.  Surgical Treatment If other therapies have not worked it may be necessary to perform surgery. As surgery may result in permanent numbness in the affected toe, doctors ten to use this procedure as a last resort. However, in most cases surgery is extremely effective. The patient usually receives a local anesthetic. Surgery involves either removing the nerve, or removing the pressure on the nerve. Two surgical approaches are possible. The dorsal approach, the surgeon makes an incision on the top of the foot, allowing the patient to walk soon after surgery, because the stitches are not on the weight-bearing side of the foot. The plantar approach, the surgeon makes an incision on the sole of the foot. In most cases the patient will be in crutches for about three weeks. The resulting scar may make walking uncomfortable. However, with this approach the neuroma can be reached easily and resected without cutting any structures. There is a small risk of infection around the toes after surgery. There are not one but two unique variations of leg length discrepancies, congenital and acquired. Congenital indicates that you are born with it. One leg is anatomically shorter than the other. As a result of developmental phases of aging, the human brain picks up on the stride pattern and recognizes some variation. Your body usually adapts by dipping one shoulder to the "short" side. A difference of under a quarter inch is not grossly excessive, demand Shoe Lifts to compensate and in most cases does not have a profound effect over a lifetime.
 Leg length inequality goes largely undiagnosed on a daily basis, however this problem is easily corrected, and can eradicate numerous instances of upper back pain. Therapy for leg length inequality commonly involves Shoe Lifts. These are generally low cost, usually priced at less than twenty dollars, in comparison to a custom orthotic of $200 if not more. Differences over a quarter inch can take their toll on the spine and should probably be compensated for with a heel lift. In some cases, the shortage can be so extreme that it requires a full lift to both the heel and sole of the shoe. Chronic back pain is easily the most common condition impacting people today. Over 80 million people experience back pain at some stage in their life. It is a problem which costs employers millions of dollars each year because of lost time and production. Innovative and better treatment methods are continually sought after in the hope of decreasing the economical influence this issue causes.  People from all corners of the world suffer from foot ache due to leg length discrepancy. In these types of cases Shoe Lifts can be of immense help. The lifts are capable of alleviating any discomfort and pain in the feet. Shoe Lifts are recommended by many experienced orthopaedic practitioners". So that you can support the body in a nicely balanced fashion, the feet have a significant role to play. Inspite of that, it's often the most overlooked area of the body. Some people have flat-feet meaning there may be unequal force exerted on the feet. This will cause other areas of the body including knees, ankles and backs to be affected too. Shoe Lifts make sure that the right posture and balance are restored. There are actually not one but two different kinds of leg length discrepancies, congenital and acquired. Congenital means that you are born with it. One leg is structurally shorter than the other. Through developmental stages of aging, the brain picks up on the stride pattern and identifies some variance. The body usually adapts by dipping one shoulder to the "short" side. A difference of less than a quarter inch isn't grossly uncommon, demand Shoe Lifts to compensate and mostly doesn't have a serious effect over a lifetime.
 Leg length inequality goes largely undiscovered on a daily basis, yet this problem is simply fixed, and can reduce many cases of lumbar pain. Treatment for leg length inequality typically involves Shoe Lifts. Most are very reasonably priced, normally being less than twenty dollars, compared to a custom orthotic of $200 or higher. When the amount of leg length inequality begins to exceed half an inch, a whole sole lift is generally the better choice than a heel lift. This prevents the foot from being unnecessarily stressed in an abnormal position. Low back pain is the most common ailment impacting men and women today. Over 80 million men and women are affected by back pain at some point in their life. It's a problem which costs businesses huge amounts of money every year due to lost time and production. New and improved treatment solutions are constantly sought after in the hope of minimizing the economic influence this issue causes.  People from all corners of the world suffer the pain of foot ache as a result of leg length discrepancy. In these types of cases Shoe Lifts are usually of very useful. The lifts are capable of eliminating any discomfort in the feet. Shoe Lifts are recommended by many experienced orthopaedic orthopedists. To be able to support the body in a well balanced fashion, feet have a crucial role to play. Despite that, it is often the most overlooked zone of the body. Some people have flat-feet meaning there may be unequal force placed on the feet. This will cause other areas of the body such as knees, ankles and backs to be affected too. Shoe Lifts make sure that correct posture and balance are restored.
Overview
 A bunion is a deformity of the metatarsophalangeal (MTP) joint at the base of the big toe. A bunion develops when the first metatarsal bone of the foot turns outward and the big toe points inward (toward the other toes), causing the joint to jut out. A bunion is most likely to develop when susceptible feet are repeatedly squeezed into narrow, pointed-toe footwear. The big toe pushes against the other toes, sometimes diving over or under them. As a result, the base of the big toe ? the metatarsophalangeal (MTP) joint ? juts or angles out from the foot. A bunion is a deformity of the metatarsophalangeal (MTP) joint at the base of the big toe. A bunion develops when the first metatarsal bone of the foot turns outward and the big toe points inward (toward the other toes), causing the joint to jut out. A bunion is most likely to develop when susceptible feet are repeatedly squeezed into narrow, pointed-toe footwear. The big toe pushes against the other toes, sometimes diving over or under them. As a result, the base of the big toe ? the metatarsophalangeal (MTP) joint ? juts or angles out from the foot.Causes Bunions can be caused by the following factors. Hereditary (especially via the female line). Rolling in (pronation) of the feet. Walking with turned out feet. Weakness of muscles controlling the big toe. Weakness of intrinsic muscles of the feet. Leaning on the big toe in a tendu, especially to second or derri?re. Reduced mobility of the big toe when on demi-pointe. Restricted pointe range. Symptoms While bunions may be considered cosmetically undesirable, they are not necessarily painful. In cases where the individual has minor discomfort that can be eased by wearing wider shoes made of soft leather and/or with the aid of spacers-padding placed between the toes to correct alignment-further treatment may not be necessary. (Anti-inflammatory agents can be used to alleviate temporary discomfort at the site of the bursa.) For those who continue to experience pain on a daily basis and who cannot wear most types of shoe comfortably, surgical treatment may be the best choice. Diagnosis Clinical findings are usually specific. Acute circumferential intense pain, warmth, swelling, and redness suggest gouty arthritis (see Gout) or infectious arthritis (see Acute Infectious Arthritis), sometimes mandating examination of synovial fluid. If multiple joints are affected, gout or another systemic rheumatic disease should be considered. If clinical diagnosis of osteoarthritic synovitis is equivocal, x-rays are taken. Suggestive findings include joint space narrowing and bony spurs extending from the metatarsal head or sometimes from the base of the proximal phalanx. Periarticular erosions (Martel sign) seen on imaging studies suggest gout. Non Surgical Treatment This is probably the most important step. Wearing the right footwear can help reduce stress on a minor deformity and reduce the likelihood of it progressing. Recommendations are that the forefoot easily fits within the width of the shoe and there is adequate cushioning and arch support. Soft materials such as smooth leather, suede or fabric will also help to reduce irritation to the area. The podiatrist plays an invaluable role in managing patients with bunions. This is because they can offer a number of options to the patient that can help relieve pain and reduce the severity of the deformity. They can also reduce pressure on skin lesions that develop as a result of the biomechanical changes. Podiatrists can prescribe customised orthotic devices that help reduce the stress on a bunion and control biomechanical factors which cause them. These may be used in conjunction with bunion splints or cushions to further offload the area. Evidence has shown a significant reduction in pain with the use of customized orthotic devices.  Surgical Treatment Procedures are designed and chosen to correct a variety of pathologies that may be associated with the bunion. For instance, procedures may address some combination of removing the abnormal bony enlargement of the first metatarsal, realigning the first metatarsal bone relative to the adjacent metatarsal bone, straightening the great toe relative to the first metatarsal and adjacent toes, realigning the cartilagenous surfaces of the great toe joint, addressing arthritic changes associated with the great toe joint, repositioning the sesamoid bones beneath the first metatarsal bone, shortening, lengthening, raising, or lowering the first metatarsal bone, and correcting any abnormal bowing or misalignment within the great toe. Connecting two parallel long bones side by side by Syndesmosis Procedure. At present there are many different bunion surgeries for different effects. The age, health, lifestyle and activity level of the patient may also play a role in the choice of procedure. Traditional bunion surgery can be performed under local, spinal or general anesthetic. In the case of laser surgery, a narcotic analgesic is typically used.[5] The trend has moved strongly toward using the less invasive local anesthesia over the years. A patient can expect a 6- to 8-week recovery period during which crutches are usually required for aid in mobility. An orthopedic cast is much less common today as newer, more stable procedures and better forms of fixation (stabilizing the bone with screws and other hardware) are used. Hardware may even include absorbable pins that perform their function and are then broken down by the body over the course of months.
Overview
 Pain of the Achilles tendon commonly affects both competitive and recreational athletes, and the sedentary. The largest tendon in the body, the Achilles tendon, endures strain and risks rupture from running, jumping, and sudden acceleration or deceleration. Overuse, vascular diseases, neuropathy, and rheumatologic diseases may cause tendon degeneration. The hallmarks of Achilles tendon problems seem to be damaged, weak, inelastic tissue. Pain of the Achilles tendon commonly affects both competitive and recreational athletes, and the sedentary. The largest tendon in the body, the Achilles tendon, endures strain and risks rupture from running, jumping, and sudden acceleration or deceleration. Overuse, vascular diseases, neuropathy, and rheumatologic diseases may cause tendon degeneration. The hallmarks of Achilles tendon problems seem to be damaged, weak, inelastic tissue.Causes The exact cause of Achilles tendon ruptures is hard to say. It can happen suddenly, without warning, or following an Achilles tendonitis . It seems that weak calf muscles may contribute to problems. If the muscles are weak and become fatigued, they may tighten and shorten. Overuse can also be a problem by leading to muscle fatigue . The more fatigued the calf muscles are, the shorter and tighter they will become. This tightness can increase the stress on the Achilles tendon and result in a rupture. Additionally, an imbalance of strength of the anterior lower leg muscles and the posterior lower leg muscles may also put an athlete at risk for an injury to the Achilles tendon. An Achilles tendon rupture is more likely when the force on the tendon is greater than the strength of the tendon. If the foot is dorsiflexed while the lower leg moves forward and the calf muscles contract, a rupture may occur. Most ruptures happen during a forceful stretch of the tendon while the calf muscles contract. Other factors that may increase the risk of Achilles tendon rupture include. Tight calf muscles and/or Achilles tendon. Change in running surface eg: from grass to concrete. Incorrect or poor footwear. A change of footwear eg: from heeled to flat shoes. It is thought that some medical conditions, such as gout, tuberculosis and systemic lupus erythematosus, may increase the risk of Achilles tendon rupture. Symptoms Tendon strain or tendon inflammation (tendonitis) can occur from tendon injury or overuse and can lead to a rupture. Call your doctor if you have signs of minor tendon problems. Minor tenderness and possible swelling increases with activity. There is usually no specific event causing sudden pain and no obvious gap in the tendon. You can still walk or stand on your toes. Acute calf pain and swelling can indicate a tear or partial tear of the Achilles tendon where it meets the calf muscle. You may still be able to use that foot to walk, but you will need to see a specialist such as an orthopedic surgeon. Surgery is not usually done for partial tears. Sometimes special heel pads or orthotics in your shoes may help. Follow up with your doctor to check for tendonitis or strain before resuming activity, because both can increase the risk of tendon rupture. Any acute injury causing pain, swelling, and difficulty with weight-bearing activities such as standing and walking may indicate you have a tear in your Achilles tendon. Seek prompt medical attention from your doctor or emergency department. Do not delay! Early treatment results in better outcome. If you have any question or uncertainty, get it checked. Diagnosis The doctor may look at your walking and observe whether you can stand on tiptoe. She/he may test the tendon using a method called Thompson?s test (also known as the calf squeeze test). In this test, you will be asked to lie face down on the examination bench and to bend your knee. The doctor will gently squeeze the calf muscles at the back of your leg, and observe how the ankle moves. If the Achilles tendon is OK, the calf squeeze will make the foot point briefly away from the leg (a movement called plantar flexion). This is quite an accurate test for Achilles tendon rupture. If the diagnosis is uncertain, an ultrasound or MRI scan may help. An Achilles tendon rupture is sometimes difficult to diagnose and can be missed on first assessment. It is important for both doctors and patients to be aware of this and to look carefully for an Achilles tendon rupture if it is suspected. Non Surgical Treatment Your doctor will advise you exactly when to start your home physical therapy program, what exercises to do, how much, and for how long to continue them. Alphabet Range of Motion exercises. Typically, the first exercise to be started (once out of a non-removable cast). While holding your knee and leg still (or cross your leg), you simply write the letters of the alphabet in an imaginary fashion while moving your foot and ankle (pretend that the tip of your toe is the tip of a pencil). Motion the capital letter A, then B, then C, all the way through Z. Do this exercise three times per day (or as your doctor advises). Freeze a paper cup with water, and then use the ice to massage the tendon area as deeply as tolerated. The massage helps to reduce the residual inflammation and helps to reduce the scarring and bulkiness of the tendon at the injury site. Do the ice massage for 15-20 minutes, three times per day (or as your doctor advises). Calf Strength exercises. This exercise is typically delayed and not used in the initial stages of rehabilitation, begin only when your doctor advises. This exercise is typically done while standing on just the foot of the injured side. Sometimes, the doctor will advise you to start with standing on both feet. Stand on a step with your forefoot on the step and your heel off the step. The heel and forefoot should be level (neither on your tip toes nor with your heel down). Lower your heel very slowly as low as it will go, then rise back up to the level starting position, again very slowly. This is not a fast exercise. Repeat the exercise as tolerated. The number of repetitions may be very limited at first. Progress the number of repetitions as tolerated. Do this exercise one to two times per day (or as your doctor advises). 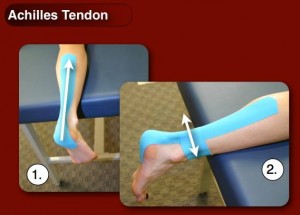 Surgical Treatment Surgical repair is a common method of treatment of acute Achilles rupture in North America because, despite a higher risk of overall complications, it has been believed to offer a reduced risk of rerupture. However, more recent trials, particularly those using functional bracing with early range of motion, have challenged this belief. The aim of this meta-analysis was to compare surgical treatment and conservative treatment with regard to the rerupture rate, the overall rate of other complications, return to work, calf circumference, and functional outcomes, as well as to examine the effects of early range of motion on the rerupture rate. |
|
